Cataracts Perth
What is a Cataract?
A cataract is a clouding of the lens in the eye. Most cataracts are seen as a normal ageing change in the eye.
What is the lens?
When we are young, the lens is a clear, flexible gel within a thin coating (lens capsule), sitting behind the iris and pupil near the front of the eye. The lens shape can be adjusted to change the focus.
In a normal eye, light passes through the transparent lens to focus clearly on the retina at the back of the eye.
If the lens is cloudy from a cataract, the image you see will be blurred.
Causes and Risk factors of Cataracts
As we age, the clear flexible gel of the lens gradually sets and hardens throughout life. This leads to restricted focus adjustment especially for near vision in those over 40 years old and over time this leads to a complete loss of the ability to vary one’s focus, affecting distance clarity as well as near vision.
Eventually, the hardening of the lens creates areas of permanent blur and opacity. This is a cataract. Over time, the cataract may extend and cloud more of the lens, making it harder to see.
Other causes also can occur:
- Secondary cataract. Cataracts can form after eye surgery for glaucoma or detached retina, diabetes or steroid use.
- Traumatic cataract. Cataracts can develop after an eye injury.
- Congenital cataract. Some babies are born with cataracts or develop them in childhood, often in both eyes.
- Radiation cataract including radiotherapy, excessive sunlight or welding.

The natural lens is not a uniform structure but has different areas with different textures. These different areas may become opaque over time or remain clear until late.
The common types include:
- Senile nuclear cataract
- Cortical cataract
- Posterior subcapsular cataract
- Posterior polar cataract
- Congenital nuclear cataract
These types can produce variations in the blur and other symptoms.
A cataract is detected through a comprehensive eye exam by your eye healthcare professional that includes:
 Visual acuity test. This eye chart test measures how well you see at various distances, both with and without spectacles.
Visual acuity test. This eye chart test measures how well you see at various distances, both with and without spectacles.- Slit-lamp biomicroscope examination to view the eyes under high magnification
- Eye health check for other eye diseases such as glaucoma, macular degeneration or optic nerve abnormality.
Your eye care professional also may do other tests to learn more about the structure and health of your eye.
Treatment
The symptoms of early cataract may be improved with new spectacles, brighter lighting, anti-glare sunglasses, or magnifying lenses.
If these measures do not help, surgery is the only effective treatment.
A cataract needs to be removed generally when blur interferes with your everyday activities, such as driving, reading, or watching TV. Surgery involves removing the cloudy lens and replacing it with an artificial lens.
Once you understand the benefits and risks of surgery, you can make an informed decision about whether cataract surgery is right for you.
In most cases, delaying cataract surgery will not cause long-term damage to your eye but can make the surgery more difficult.
If you require surgery, your optometrist or GP will refer you to a specialist eye surgeon (ophthalmologist) to remove the cataract.
If you have cataracts in both eyes that require surgery, the surgery will typically be performed on one eye at a time, usually one to two weeks apart or longer.
Manual phacoemulsification lens extraction is performed by creating a small (less than 2.5mm) incision at the edge of the cornea (the clear, dome-shaped window at the front of the eye). Your surgeon manually tears a circular opening in the capsule (coating) of the lens, then inserts a small device through the incision that uses ultrasonic vibration to soften and break up the hardened lens, so that it can be removed by suction. Most cataract surgery today is done by phacoemulsification, also called “small incision cataract surgery” or just “phaco”.
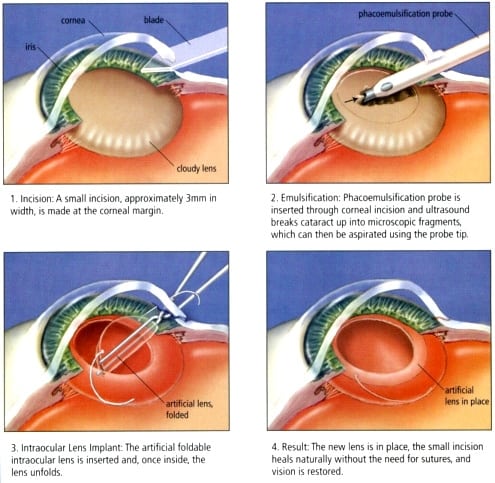
After the natural lens has been removed, it typically is replaced by an artificial lens, called an Intra-Ocular Lens (IOL).
An IOL is a clear, soft plastic lens (like a soft contact lens) that becomes a permanent part of your eye, focussing light clearly onto the retina, improving your vision. You will not feel or see the new lens and no maintenance is required.

As with any surgery, cataract surgery poses some risks, such as infection and bleeding. After surgery, you must keep your eye clean, wash your hands before touching your eye, and use the prescribed medications to help minimize the risk of infection. Serious infection can result in loss of vision.
Some inflammation within the eye is normal after surgery but may be prolonged and the use of anti-inflammatory eye drops is routine post-operatively.
Cataract surgery minimally increases your risk of retinal detachment. Other eye disorders, such as high myopia (extreme near-sightedness), can further increase your risk of retinal detachment after cataract surgery. One sign of a retinal detachment is a sudden increase in flashes or floaters. Floaters are little “cobwebs” or specks that seem to float about in your field of vision. Any vision change or vision loss should be reported to your surgeon.
Talk to your eye care professional about these risks. Make sure cataract surgery is right for you.
Before surgery, your doctor will need to do some tests. These tests include measuring your eye for the correct intraocular lens refractive power for best-unaided focus. This information helps your doctor choose the right type of IOL.
You will be advised to fast the day of surgery.
At the hospital or eye clinic, medicated eye drops will be put into your eye to dilate the pupil. The area around your eye will be washed and cleansed with an antiseptic.
The operation usually lasts less than 30 minutes and is almost painless. Many people choose to stay awake during surgery. Others may need to be put to sleep for a short time.
If you are awake, you will have an anaesthetic eye drop to numb your eye. Some light, calming sedation is provided by the anaesthetist.
After the operation, a patch or clear plastic shield may be placed over your eye. You will rest for a short while. Your medical team will watch for any problems, such as bleeding.
Most people who have cataract surgery can go home the same day. You will need someone to drive you home.
Pain is unusual after cataract surgery, but the itching and mild discomfort are normal. Some watery discharge is also common. Your eye may be sensitive to light and touch. If you have discomfort, your doctor can suggest treatment. After one or two days, most discomfort should disappear.
For a few weeks after surgery, your doctor may ask you to use eye drops to help to heal and decrease the risk of infection. Avoid rubbing or pressing on your eye.
When you are home, avoid stooping from the waist to pick up objects on the floor or anything that may place pressure on the eye. Do not lift any heavy objects. You can walk, climb stairs, and do light household chores.
In most cases, healing will be complete within four to six weeks. Your doctor will schedule exams to check on your progress.
Problems after surgery are rare, but they can occur.
Sometimes the lens capsule that encloses the IOL becomes thickened and may blur your vision. This condition is called capsule opacification. This can develop months or even years after successful lens replacement surgery and is treated with a laser. Your doctor uses a laser to clear the opacity with a clinic procedure called a YAG laser capsulotomy performed under local anaesthetic eye drops. It is painless but rarely can result in increased eye pressure or other eye problems. Treatment rarely needs to be repeated.
You can return quickly to many everyday activities, but your vision may still have a slight blur until healed. The healing eye needs time to adjust so that it can focus properly with the other eye, especially if the other eye has a different focus or has a cataract. Ask your doctor when you can resume driving.
If you received an IOL, you may notice that the colours are very bright. The IOL is clear, unlike your natural lens that may have had an age-related yellowish/brownish tint. Within a few months after receiving an IOL, you will become used to improved colour vision.
Also, when your eye heals, you may need to update your glasses for the new focus for distance or reading.

 Visual acuity test. This eye chart test measures how well you see at various distances, both with and without spectacles.
Visual acuity test. This eye chart test measures how well you see at various distances, both with and without spectacles.